Pharmacists embrace new DRG code for stroke
Hospitals often take a financial beating when they do not get adequately reimbursed for certain high-priced, lifesaving drugs. But thanks to a new diagnostic code for stroke patients, which goes into effect on Oct. 1, 2005, reimbursement for critical clot-busting drugs (thrombolytics) will be more equitable.
The Centers for Medicare & Medicaid Services has created a new diagnostic code to reimburse hospitals at a higher rate for acute ischemic stroke patients who are treated with clot-busting agents.
The new category, known as diagnosis related group (DRG) 559, will reimburse hospitals $11,578 for a patient treated for acute ischemic stroke with a clot-busting drug. Prior to the new DRG code, reimbursement was limited to $4,000 to $6,000. The new code, said William Gouveia, director of pharmacy at Tufts-New England Medical Center in Boston, is encouraging for hospitals that have essentially been giving these drugs away. Reimbursement has not been good, and hospitals have been taking it on the chin, he said.
Gerald Meyer, Pharm.D., assistant director of pharmacy at Thomas Jefferson University Hospital in Philadelphia, welcomed the new DRG code for stroke patients and noted that reimbursement issues related to expensive drugs and devices are always a challenge and that it usually takes time to get reimbursement levels set properly. "But when you have therapies for which the evidence suggests it is appropriate, then the reimbursement should be reasonable and appropriate."
Medical experts claim that the new code will provide hospitals with appropriate reimbursement for the higher costs related to the treatment of ischemic-stroke patients-a significant development considering that treating patients with a clot-busting drug is more expensive, based on the need for increased patient monitoring, additional personnel, and higher lab and pharmacy costs.
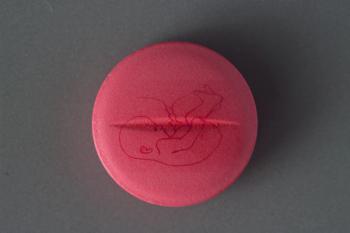
CMS contends that the change in DRG coding for stroke is not to award higher payment for a specific drug but rather to recognize the need for overall care for stroke patients as a group. CMS' goal is to make payment relate more closely to resource use, and to recognize that the use of thrombolytic agents, such as the tissue plasmino-gen activator (tPA) Activase (alteplase, Genentech), in a carefully selected patient population, will lead to better outcomes and may lessen the need for post-acute care. In response to CMS' action, Genentech reported that it does not expect the DRG change to have an impact on tPA sales. However, company officials said that it's too early to determine the ultimate effect.
Several organizations-including the American Stroke Association and the Brain Attack Coalition-urged CMS to make the DRG change. Stroke is the third-highest cause of death in the nation as well as a leading cause of disability, afflicting more than 700,000 people annually in the United States. In addition, 15% to 30% of stroke survivors are left permanently disabled.
Further information about DRG 559 can be found at CMS' Web site:
Newsletter
Pharmacy practice is always changing. Stay ahead of the curve with the Drug Topics newsletter and get the latest drug information, industry trends, and patient care tips.