- Drug Topics March 2023
- Volume 167
- Issue 03
Mind-Body Resilience for Women: A Focus on Depression
Developing innovative solutions for women with depression, accounting for differences in gender and sex, are critically important
Depression is the leading cause of disability and a major contributor to the overall global burden of disease.1 But as the Lancet World Psychiatric Association Commission pointed out in its 2022 report on depression, despite how common depression is across the life course, critical barriers have prevented depression from receiving sufficient resources and global attention.1
Depression has historically been stigmatized and misunderstood. The condition arises due to a combination of biological, social, and psychological factors, and limited access to treatment and a lack of cross-disciplinary, collaborative research and care has hindered progress. Additionally, women are disproportionately affected by depression and are twice as likely to have a diagnosis of depression compared with men, likely due to a combination of health inequities, gender biases, and biological factors.1 Depression is also a risk factor to develop dementia in older adults, and it might be a reason more women have dementia than men.2 Developing innovative solutions for depression—especially those focused on women that account for sex and gender differences—are critical to improving individual and collective resilience.
To develop women-centered solutions for depression, it is important to understand the various factors that contribute to women’s greater risk for depression, and a health equity and public health lens is imperative. The distinction between sex and gender also needs to be clear, with sex referring to biological differences and gender encompassing socially constructed and enacted roles and behaviors shaped by historical and cultural contexts. Additionally, diagnostic tools, symptom screeners, medications, and other health tools must not have sex or gender bias.
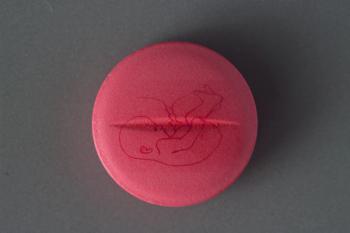
Women in their reproductive years undergo cycle changes in steroid hormones (progesterone/ estrogen) over the menstrual cycle. The role of these changes as a factor contributing to depression and mood changes is seen in women with premenstrual dysphoric disorder (PMDD) and premenstrual syndrome (PMS). The estimated prevalence in reproductive women is 5% and 20%, respectively. There is growing evidence that the rise in ovarian steroid hormone production and the effect of their metabolites (allopregnanolone in particular) on central brain receptors as progesterone receptor modulators contribute to the mood symptoms in PMDD and PMS.3 More research is needed to understand the long-term neurological impacts of birth control and hormone therapy.4 Treatments are now being developed to target these newer proposed actions of hormones on the central brain systems with either suppressing ovarian function (removing the natural fluctuations in hormones) or “correcting” the neurotransmitter or neurosteroid dysregulation with the use of targeted specific antidepressants.5,6
The preponderance of depression in women occurs largely during the reproductive years, is not evident before puberty, and is less marked after menopause. Societal factors may also play an important role; even in developed countries, women still often take a greater responsibility for child rearing and domestic activities while still being expected to progress their careers— known as a “double day.” Women worldwide are also the majority of caregivers for family members needing health care; often this role is unpaid.
Intimate Partner Violence
Depression is also linked to intimate partner violence (IPV). One in 3 women around the world have experienced physical or sexual IPV.7 Since the start of the COVID-19 pandemic, IPV has escalated and been called a shadow pandemic by the United Nations. In some countries, there has been a 300% increase in police reports of IPV, likely fueled by COVID-19 effects and mitigation strategies.8 UN Women projected that for every 3 months of lockdown, an additional 15 million women would be affected by IPV.9
One particularly devastating yet unaddressed and long-neglected impact is the mental and physcial health effects of IPV, including traumatic brain injury (TBI) and depression. Numerous studies have found that women exposed to IPV are more likely to develop depression than women who are not exposed.10 This finding is not surprising, given that mental health issues are common sequelae of brain injury that may emerge and worsen years after injury. However, IPV is too often left out of conversations around prevention and treatment of depression.
Chronic Health Conditions
It is also important to note the connection in women between depression and chronic health conditions such as heart disease. Since 1984, heart disease has been the leading cause of death for women in the US.11 Women are also more likely than men to die after a heart attack,11 and are more likely to be undiagnosed, misdiagnosed, or poorly treated for heart disease due to pervasive bias and the male body being the default model for biomedical care and research.
Additionally, the Guidelines for the Prevention of Cardiovascular Disease in Women by the American Heart Association show the profound impact of hypertension, diabetes, and depression on women’s hearts.12 It is imperative to understand the huge impact of psychosocial risk factors on women’s hearts and address problems including depression and social isolation.12
Dementia
Understanding the role of depression in dementia for women is also imperative. The WHAM Report (Women’s Health Access Matters) found that women comprise 66% of the nearly 7 million individuals in the United States with Alzheimer disease (AD), and yet only 12% of the 2019 NIH AD fund went to projects focused on women.13
Even more crucially, the report demonstrated the following:
-Doubling the funds for women’s AD research pays for itself 3 times over. This 224% return on investment adds 15% more to our economy than general AD research
-Adding $300 million for research on women generates $930 million in economic gains, adds back 4000 years of life, eliminates 6500 cases of AD and related dementias, and saves 3500 years of nursing home care and costs.
-Depression is one of the largest modifiable risk factors for dementia.14 Thus, understanding the link between depression and dementia and accounting for depression in dementia prevention strategies in women is essential.14
Solutions
Novel initiatives focused on women can reduce the impact of depression and increase global resilience. As a recent Rock Health report finds, women’s health solutions often remain siloed to pregnancy and reproductive-related issues.15 There is a dearth of women-focused solutions for chronic health and behavioral health and an even larger gap for solutions at the intersection of both.15 Solutions that include technology, drug development, and devices are urgently needed, and convergence solutions that combine multiple domains and technologies, such as blending platform and frontier technologies, are key.
Developing these solutions is not only a medical and moral imperative; there is also a significant economic and commercial upside. Emergen Research projects that the global market for women’s health will reach $60 billion in 2027.16 Additionally, women are the chief medical officers of society, controlling 80% of health care decisions in the US and spending 29% more per capita on health care than men.17,18
By developing women-focused solutions for depression that account for various factors, including the relationship between depression, heart disease, and dementia, we can build a more resilient society and world.
References
1. Herrman H, Patel V, Kieling C, et al.
2. Barnes DE, Yaffe K, Byers AL, et al.
3. Lanza di Scalea T, Pearlstein T.
4. Savolainen-Peltonen H, Rahkola-Soisalo P, Hoti F, et al.
5. Schmidt PJ, Martinez PE, Nieman LK, et al.
6. Hantsoo L, Grillon C, Sammel M, et al.
7. Breiding MJ, Smith SG, Basile KC, et al.
8. Valera EM.
9. Mlambo-Ngcuka P. Gender-based violence: we must flatten the curve of this shadow pandemic. November 25, 2020. Accessed May 12, 2022.
10. Ellsberg M, Jansen HAFM, Heise L, et al.
11. Mehta LS, Beckie TM, DeVon HA, et al.
12. Mosca L, Benjamin EJ, Berra K, et al.
13. Baird MD, Zaber MA, Dick AW, et al. Societal Impact of Research Funding for Women’s Health in Alzheimer’s Disease and Related Dementias. Rand Corporation; 2021.
14. Livingston G, Huntley J, Sommerlad A, et al.
15. DeSilva J, Krasniansky A. Building comprehensive women+ digital health: Eight sectors serving women+ needs. Rock Health. September 27, 2021. Accessed May 12, 2022.
16. Femtech Market By Type (Devices, Software, Services), By End-Use (Direct-to-Consumer, Hospitals, Fertility Clinics, Surgical Centers, Diagnostic Centers), By Application (Reproductive Health, Pregnancy & Nursing Care, Pelvic & Uterine Healthcare), By Region, Forecasts to 2027. EMERGEN Research. June 2021. Accessed May 12, 2022.
17. Femtech—time for a digital revolution in the women’s health market. Frost & Sullivan. January 31, 2018. Accessed May 12, 2022.
18. Gambon E, Stotz C, Sandhu N. Femtech is expansive—it’s time to start treating it as such. Rock Health. August 3, 2020. Accessed May 12, 2022.
Articles in this issue
almost 3 years ago
Azithromycin Reduces Risk of Maternal Sepsis, Death in Vaginal Deliveryalmost 3 years ago
Show Them The Moneyalmost 3 years ago
Cancer Risk Associated With UV Nail Dryersalmost 3 years ago
Racial, Ethnic Inequities Persist in Diabetes Carealmost 3 years ago
Pharmacists Are Crucial in Managing Endometriosis Symptomsalmost 3 years ago
The Role of the Pharmacist in Cannabis LegalizationNewsletter
Pharmacy practice is always changing. Stay ahead of the curve with the Drug Topics newsletter and get the latest drug information, industry trends, and patient care tips.