- Drug Topics July/August 2023
- Volume 167
- Issue 07
Inside Insomnia: Pharmacist Management of Sleep Disorders
Digging deeper into the cause of insomnia and counseling patients on lifestyle changes can help improve their sleep health.
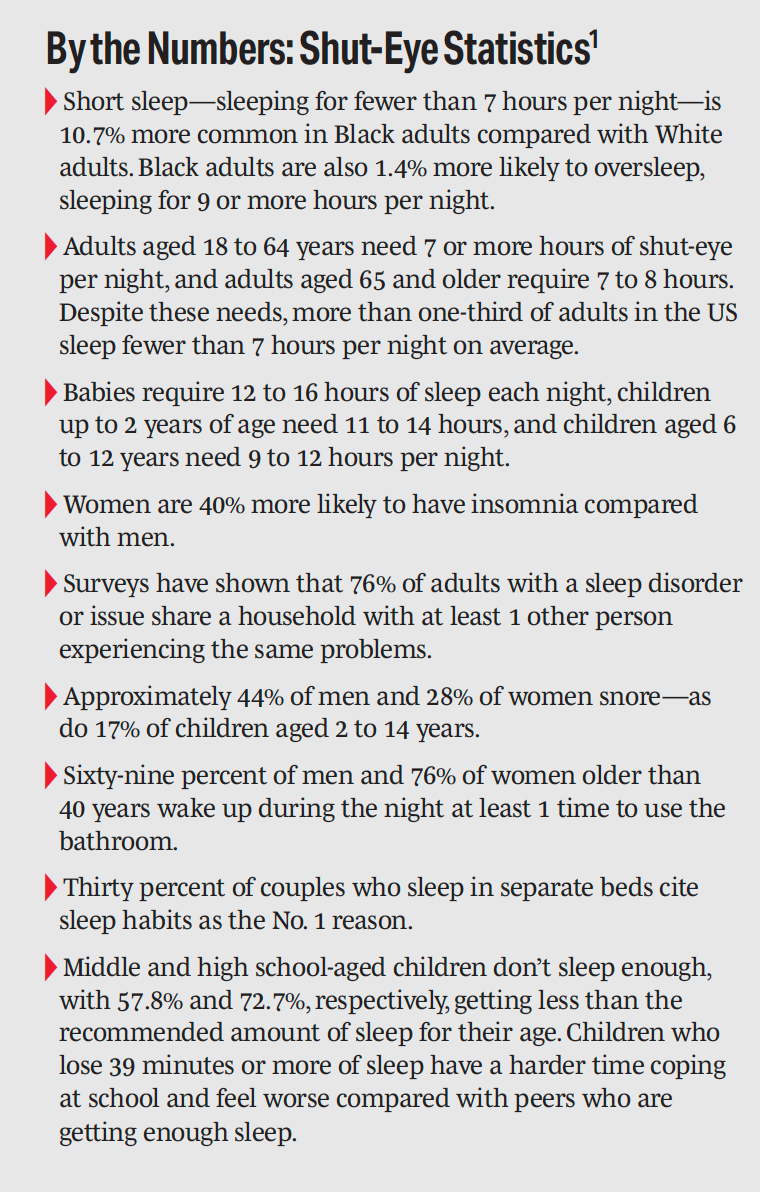
Approximately 70 million individuals in the United States live with ongoing sleep disorders, and nearly 15% of all US adults have insomnia.1 These are troubling numbers, particularly because insomnia can impact the way an individual functions throughout the day, impairing their ability to work, drive, and perform nearly all daily activities. For patients with insomnia, turning to their pharmacist can be a good first step in combatting sleep disorders and getting the rest they need.
Farah Khorassani, PharmD, an associate clinical professor at the University of California, Irvine School of Pharmacy and Pharmaceutical Sciences, noted that pharmacists play a crucial role in educating patients about good sleep habits—also known as sleep hygiene—as well as in identifying medications or substances that could be contributing to insomnia; recommending medications and doses for insomnia; providing clinician education on the risks, benefits, and evidence on the use of different agents; and counseling patients on the use of these medications.
There are 5 benzodiazepines that are FDA approved for insomnia: estazolam (Prosom), flurazepam (Dalmane), quazpam (Doral), temazepam (Restoril), and triazolam (Halicon). Pharmacists can counsel patients on the use of these prescribed medications, but for many patients, insomnia can be mitigated through lifestyle modifications and appropriate sleep hygiene. “According to the CDC, some examples of good sleep hygiene include going to sleep and waking up at a consistent time every day, removing electronic devices from the bedroom, keeping the a comfortable temperature, exercising during the day—but not too late because that can keep you awake later—and avoiding large meals, caffeine, and alcohol too close to bedtime,” Khorassani explained.
Kathy M. Campbell, PharmD, has been an independent pharmacist for more than 30 years in Owasso, Oklahoma, and has served 4 generations of patients, many of whom have sleep issues and insomnia. Campbell noted that traditionally on the medication side, pharmacists are helping customers manage their prescriptions or triaging the issues even before someone goes to see their primary care provider.
“They may tell me they have some sleep issues and ask what they should be taking, but I tend to look more at why they are having issues of sleep,” Campbell explained. “When a patient comes to me about that, [I always do] a deeper triage as to what could be the source of the insomnia.” The 2 biggest culprits she sees are low oxygen or sleep apnea keeping the patient awake or glucose irregularities. “There are some tools patients can use, such as sleep apps like a Fitbit, [so] they can see the changes in their sleep and monitor to see if the blood pressure or heart rate accelerates—which are symptoms of not having good oxygenation,” Campbell said. “Nothing freaks the brain out like no oxygen. If you don’t have enough oxygen, your body will wake you up.”
In those instances, Campbell will refer the patient to a sleep study or to their primary care provider to talk more about other options.
Josh Rimany, RPh, FACA, founder and chief wellness officer of Dilworth Wellness Center in Charlotte, North Carolina, likes to be known as the “pharmacist who goes beyond the pill” because he takes a wellness-oriented approach in his practice, focusing on moving away from medication dependency. When he works with a patient who has a sleep issue, his first course of action is to talk about the importance of sleep and ask questions about the “why” and the lifestyle choices that may be contributing to the problem.
“Seventy million people don’t get enough sleep, and the CDC considers it a public health problem, yet only 43% of providers talk to their patients about sleep,” Rimany said. “Sleep is considered one of the No. 1 tools for longevity. If we’re going to bring vibrant life into people, nailing 7 to 8 hours of quality sleep is very important.”
OTC Options
The pharmacist can also advise patients and customers on OTC options to help with sleep—such as melatonin or antihistamines—including the benefits and potential adverse effects of each medication. Counseling is where a pharmacist’s expertise really shines.
The OTC options available to a patient depend on various factors, including their comorbid conditions and the duration of insomnia, Khorassani explained. “In my opinion, melatonin is a good starting point because of its tolerability profile,” she said. “It is an OTC supplement that is safe to use in most patients with insomnia. It is also non–habit forming so can be taken long term and has few adverse effects. The evidence for its efficacy is not very strong, but anecdotally, many patients have told me it helped their insomnia.”
Other agents such as diphenhydramine HCI (Benadryl) and doxylamine (Unisom) are also options, but they come with more adverse effects than melatonin, such as dry mouth and next-day drowsiness. Because of this, these agents are best used for short-term insomnia only.2
It is important for pharmacists to assess the patient’s individual needs and consider any comorbidities or medications that may impact sleep. They can also refer patients to a sleep specialist if necessary.
“I’ve had a few patients who have complained of insomnia because they were taking [the antidepressant bupropion (Wellbutrin)], which can cause insomnia,” Khorassani said. “Several of them were taking it twice daily and were taking the second dose at bedtime. If this medication is taken twice daily, the second dose is ideally given before 4 PM because of its stimulating properties.
“Talking to patients about the timing of their medication helped me uncover a way to improve their insomnia. By suggesting they switch the medication to earlier in the day, their sleep improved, and they didn’t require any additional medication.”
Implementing Lifestyle Changes
Poor sleep is linked to several chronic diseases and can also raise the risk of developing Alzheimer disease, depression, dementia, obesity, anxiety, and more—including premature death.3
“That really gets patients’ attention,” Rimany said. “You can give them tricks and tips for lifestyle habits all day long, but they generally won’t adopt them unless it’s really important to them. When I talk to patients about sleep on a pharmacy level— and this is something I’ve researched quite a bit—there is [an] increase in mortality rate for people who take sleep medication on a regular basis.”4
Sleep should be prioritized for a long life, and pharmacists can also help patients manage sleep concerns by recommending nonpharmacological interventions such as cognitive-behavioral therapy for insomnia. Other lifestyle modifications include reducing caffeine intake, avoiding the use of electronics before bedtime, and establishing a consistent sleep routine, all before turning to prescription medications.
Campbell will occasionally recommend melatonin but said she is more concerned about a patient’s sleep hygiene. Before melatonin, she will remind patients to ensure that their bedroom is optimized for sleep and that they aren’t eating too close to bedtime or drinking too much alcohol.
“If they are at the age where they are not producing as much melatonin as they need, I will put them on a very low-dose melatonin,” she said. “I incorporate a lot of nutrition science and a lot of stress science into how I approach and coach patients.”
One factor that has contributed to poor sleep over the past decade is our use of social media. Campbell emphasized the importance of reminding patients to disconnect from their devices well before bedtime.
Another sleep disruptor? Our pets. Individuals who sleep with their pets or who are routinely awoken by their pets during the night experience poor sleep. “Sleep is when the brain and the body recover and rebuild, and sleep is so critical to long-term health,” Campbell said. “Tolerating interruptions is going to alter your long-term health and longevity.”
Rimany offers his customers plenty of options for help and is always looking to educate them more about the benefits of sleep and ways to combat their sleep issues. “A ‘Pharmacy 2.0’ that wants to go beyond dispensing will look at the lifestyle—diet, supplements, and labs—to figure out the best plan,” he said. “Consistency matters [and] quality matters….Cutting out stimulants during the evening and keeping the room at 68 degrees or less [can all help. Some people even use weighted blankets.”
Rimany advises patients to set a cutoff of 2 hours before bedtime for eating or drinking anything other than water, explaining that if the body is digesting, it’s not working toward resting. “Working out is also not a great thing to do before bed,” he said. “Screen time is obviously huge because the blue light and LED lights emitted from these devices are telling your eyeballs that it’s noon, so your brain doesn’t let your body settle down. Blue light–blocking glasses are very important in these cases.” Complete dark—with blackout curtains, if necessary—is also crucial to managing insomnia because any sliver of light can wake up the body’s clock.
For patients who wake up and can’t fall back asleep in 5 minutes, “It’s actually healthier [for them] to get out of bed and read, or do something quiet to get tired,” Rimnay said. “I’m a big fan of meditation and winding myself down. [Putting thoughts down into] a journal can also help [patient’s] get their brain more rested.”
References
1. Suni E, Truong K. Sleep statistics. Sleep Foundation. Updated May 18, 2023. Accessed June 29, 2023. https:// www.sleepfoundation.org/how-sleep-works/sleep-facts-statistics
2. Olson EJ. Adult health. December 9, 2021. Accessed July 11, 2023. https://www.mayoclinic.org/healthy-lifestyle/adult-health/expert-answers/sleep-aids/faq-20058393
3. What are sleep deprivation and deficiency? National Heart, Lung, and Blood Institute. Updated March 24, 2022. Accessed July 11, 2023. https://www.nhlbi.nih.gov/health/sleep-deprivation
4. Sun Y, Tsai MK, Wen CP. Association of sleep duration and sleeping pill use with mortality and life expectancy: a cohort study of 484,916 adults. Sleep Health. 2023;9(3):354-362. doi:10.1016/j.sleh.2023.01.017
Articles in this issue
over 2 years ago
FDA Approves Sotagliflozin for Treatment of Heart Failureover 2 years ago
New Treatment Approved for Menopausal Hot Flashesover 2 years ago
Here’s a Tip: More Money Is the Solutionover 2 years ago
2023-2024 Flu Season: What to Expectover 2 years ago
Utilizing AI for Medication Managementover 2 years ago
Pharmacists Applaud New Bionic Pancreas for Type 1 Diabetesover 2 years ago
ASHP: Adalimumab Biosimilar Pipeline ReviewNewsletter
Pharmacy practice is always changing. Stay ahead of the curve with the Drug Topics newsletter and get the latest drug information, industry trends, and patient care tips.